Soap Note Examples: Master Documentation

Soap notes are a crucial part of medical documentation, providing a clear and concise way to record patient information, treatment plans, and outcomes. The Soap note format, which stands for Subjective, Objective, Assessment, and Plan, has been widely adopted in the healthcare industry due to its effectiveness in promoting accurate and efficient documentation. In this article, we will delve into the world of Soap note examples, exploring their significance, components, and best practices for master documentation.
Introduction to Soap Notes

Soap notes were first introduced in the 1960s by Dr. Lawrence Weed, a physician who recognized the need for a standardized method of documentation. The Soap note format was designed to improve the quality and clarity of medical records, making it easier for healthcare professionals to communicate patient information and develop effective treatment plans. Today, Soap notes are used in a variety of healthcare settings, including hospitals, clinics, and private practices.
Components of a Soap Note
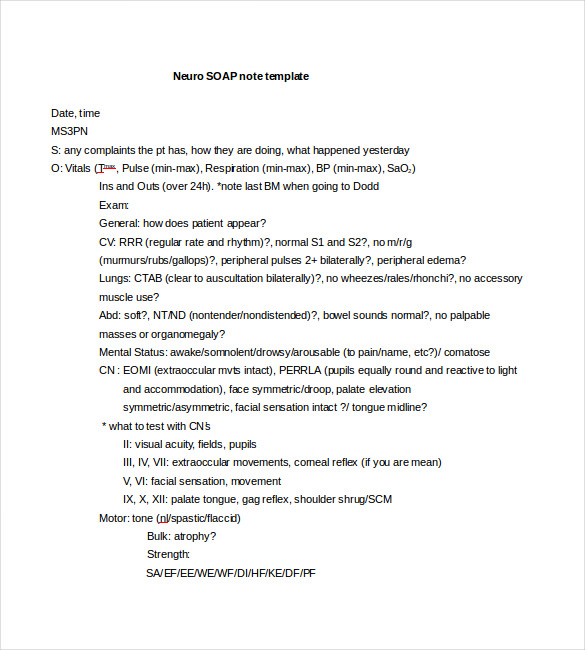
A typical Soap note consists of four main components: Subjective, Objective, Assessment, and Plan. Each component plays a critical role in the documentation process, providing a comprehensive overview of the patient’s condition and treatment.
The Subjective component includes the patient's personal account of their symptoms, medical history, and concerns. This information is typically gathered through patient interviews and questionnaires. The subjective section of the Soap note provides valuable insights into the patient's experiences and perceptions, helping healthcare professionals to better understand their needs and develop personalized treatment plans.
The Objective component includes measurable data and observations, such as vital signs, laboratory results, and physical examination findings. This information is used to support the patient's subjective reports and provide a more complete picture of their condition. The objective section of the Soap note is essential for developing accurate diagnoses and treatment plans.
The Assessment component includes the healthcare professional's diagnosis and evaluation of the patient's condition. This section summarizes the key findings from the subjective and objective components, highlighting the patient's strengths, weaknesses, and areas for improvement. The assessment section of the Soap note provides a clear and concise summary of the patient's condition, serving as a foundation for the development of effective treatment plans.
The Plan component outlines the treatment plan and interventions, including medications, therapies, and lifestyle modifications. This section provides a clear direction for patient care, ensuring that all healthcare professionals involved in the patient's care are aware of the treatment goals and objectives. The plan section of the Soap note is essential for promoting continuity of care and achieving optimal patient outcomes.
| Soap Note Component | Description |
|---|---|
| Subjective | Patient's personal account of symptoms, medical history, and concerns |
| Objective | Measurable data and observations, such as vital signs and laboratory results |
| Assessment | Diagnosis and evaluation of the patient's condition |
| Plan | Treatment plan and interventions, including medications and therapies |

Best Practices for Master Documentation
Master documentation requires attention to detail, organization, and clarity. When creating Soap notes, healthcare professionals should adhere to the following best practices:
Use Standardized Terminology
Using standardized terminology is essential for ensuring that Soap notes are clear and concise. Healthcare professionals should use widely accepted medical terms and abbreviations, avoiding ambiguity and confusion.
Be Concise and Focused
Soap notes should be concise and focused, providing only the most relevant information. Healthcare professionals should avoid including unnecessary details or information that is not relevant to the patient’s condition or treatment plan.
Use a Standardized Format
Using a standardized format for Soap notes helps to promote consistency and clarity. Healthcare professionals should use the Soap note format, including the subjective, objective, assessment, and plan components, to ensure that all relevant information is included.
Review and Update Regularly
Soap notes should be reviewed and updated regularly to ensure that they remain accurate and relevant. Healthcare professionals should review the patient’s medical history, treatment plan, and progress, making updates as necessary to reflect changes in the patient’s condition or treatment.
Conclusion
In conclusion, Soap notes are a vital part of medical documentation, providing a clear and concise way to record patient information, treatment plans, and outcomes. By understanding the components of a Soap note and following best practices for master documentation, healthcare professionals can promote effective communication, collaboration, and patient care. Whether you are a seasoned healthcare professional or just starting your career, mastering the art of Soap note documentation is essential for delivering high-quality patient care and achieving optimal outcomes.
What is the purpose of a Soap note?
+
The purpose of a Soap note is to provide a clear and concise way to record patient information, treatment plans, and outcomes. It helps healthcare professionals to communicate effectively, develop personalized treatment plans, and achieve optimal patient outcomes.
What are the components of a Soap note?
+
The components of a Soap note include the subjective, objective, assessment, and plan. The subjective component includes the patient’s personal account of their symptoms, medical history, and concerns. The objective component includes measurable data and observations, such as vital signs and laboratory results. The assessment component includes the diagnosis and evaluation of the patient’s condition, and the plan component outlines the treatment plan and interventions.
Why is standardized terminology important in Soap notes?
+
Standardized terminology is important in Soap notes because it helps to ensure that the information is clear and concise, avoiding ambiguity and confusion. It also promotes effective communication and collaboration among healthcare professionals, ultimately improving patient outcomes.


