10+ Pvc Icd 10 Tips For Accurate Diagnosis

The diagnosis and coding of Premature Ventricular Contractions (PVCs) can be complex, requiring a thorough understanding of both the clinical presentation and the ICD-10 coding system. PVCs are a type of arrhythmia characterized by early electrical impulses originating in the ventricles, causing the heart to contract prematurely. Accurate diagnosis and coding are crucial for effective patient care, insurance reimbursement, and healthcare statistics. Here are 10+ tips for accurate diagnosis and coding of PVCs using ICD-10:
Understanding PVCs and ICD-10 Basics
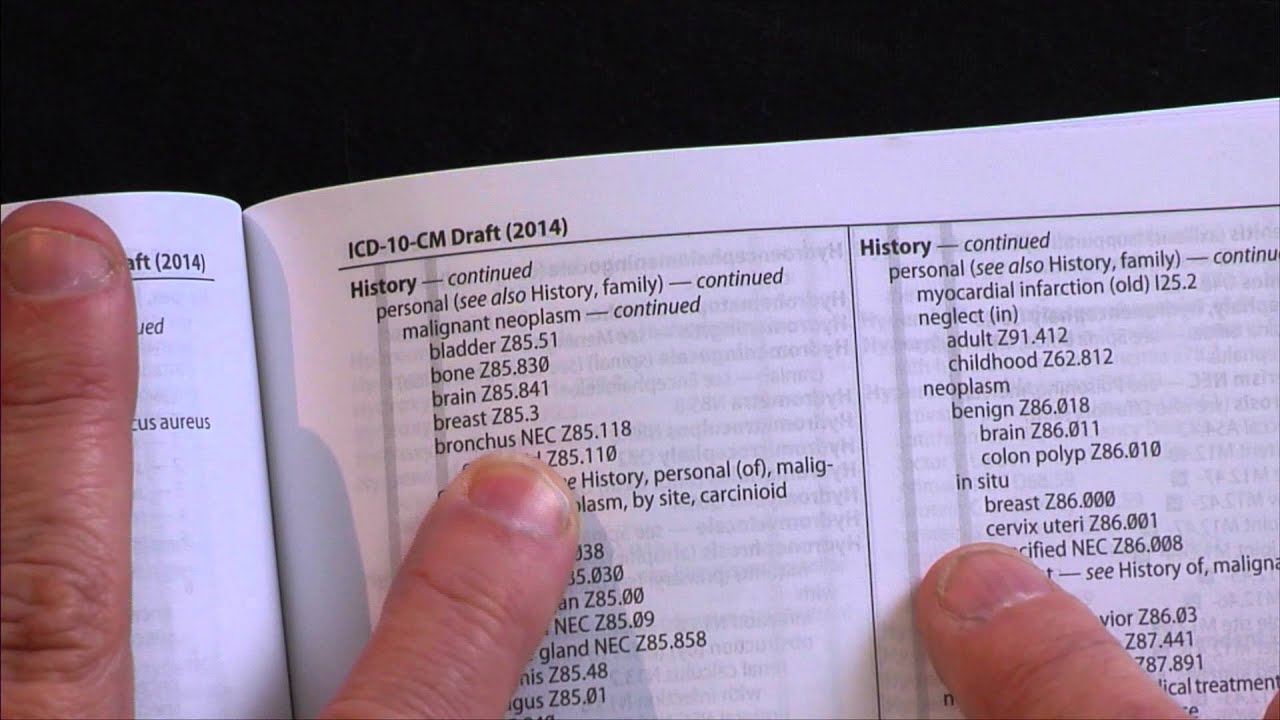
ICD-10, or the International Classification of Diseases, Tenth Revision, is a system used worldwide to code and classify diseases, symptoms, and procedures. For PVCs, the relevant codes fall under the category of arrhythmias. It’s essential to understand that ICD-10 codes are very specific, often requiring detailed information about the condition, including its cause, severity, and any associated symptoms or complications.
Tip 1: Identify the Correct Code Category
PVCs are typically coded under the category “I49” in ICD-10, which pertains to other cardiac arrhythmias. However, the specific code used can vary depending on whether the PVCs are specified as premature ventricular contractions or if they are part of a broader diagnosis such as ventricular tachycardia or bigeminy.
Tip 2: Specify the Type of Arrhythmia
It’s crucial to specify the type of arrhythmia. For PVCs, the code I49.3 (Premature ventricular contractions) is often used. However, if the PVCs are part of a more complex arrhythmia or if they lead to other conditions like ventricular fibrillation, a different code may be more appropriate.
Tip 3: Consider Associated Conditions
PVCs can be associated with other cardiac conditions or may be a symptom of an underlying heart disease. ICD-10 coding allows for the reporting of multiple diagnoses, so it’s essential to code not just the PVCs but also any related conditions, such as heart failure or coronary artery disease.
Tip 4: Use Additional Codes for Symptoms
If the PVCs are causing symptoms such as chest pain, shortness of breath, or palpitations, these should be coded separately. Symptoms can provide valuable information for patient care and can impact the coding of the primary diagnosis.
Tip 5: Document Laterality and Specificity
ICD-10 often requires laterality (which side of the body is affected) and specificity (the exact nature of the condition). While PVCs typically do not require laterality, specifying whether the condition is acute or chronic can be crucial for accurate coding and patient care.
Tip 6: Review Coding Guidelines
ICD-10 coding guidelines are regularly updated, and it’s essential to stay current with these changes. Guidelines can provide clarification on coding complex conditions and ensure that codes are used consistently across different healthcare settings.
Tip 7: Utilize Coding Resources
Several resources are available to help with ICD-10 coding, including coding manuals, online databases, and professional coding organizations. These resources can provide detailed information on codes, including examples of when to use them and how to sequence them.
Tip 8: Consider the Impact of Coding on Patient Care
Accurate ICD-10 coding not only affects reimbursement and statistics but also impacts patient care. Codes can influence treatment decisions, and accurate documentation of PVCs and related conditions can ensure that patients receive appropriate care.
Tip 9: Stay Updated on Clinical Knowledge
Understanding the clinical aspects of PVCs, including their causes, diagnosis, and treatment, is essential for accurate coding. Staying current with clinical guidelines and research can help ensure that coding reflects the best practices in patient care.
Tip 10: Engage in Continuous Education
Both coding professionals and healthcare providers should engage in continuous education to stay updated on ICD-10 codes, clinical practices, and any changes to guidelines or coding conventions.
Tip 11: Use Technology to Aid in Coding
Technology, such as electronic health records (EHRs) and coding software, can aid in accurate and efficient ICD-10 coding. These tools can provide real-time coding assistance, reduce errors, and help ensure compliance with coding guidelines.
| ICD-10 Code | Description |
|---|---|
| I49.3 | Premature ventricular contractions |
| I49.0 | Ventricular fibrillation and flutter |
| I49.1 | Ventricular tachycardia |
| I49.2 | Ventricular rhythm disturbance, unspecified |
| I49.4 | Other specified cardiac arrhythmias |
| I49.5 | Unspecified cardiac arrhythmia |

What is the most common ICD-10 code used for premature ventricular contractions (PVCs)?
+The most common ICD-10 code for PVCs is I49.3, which specifically denotes premature ventricular contractions.
Do I need to code symptoms associated with PVCs separately?
+Yes, symptoms such as chest pain, shortness of breath, or palpitations should be coded separately from the PVCs themselves. This provides a more comprehensive picture of the patient’s condition and can impact treatment decisions.
Where can I find resources to help with ICD-10 coding for cardiac arrhythmias?
+Resources for ICD-10 coding include official coding manuals, online databases, professional coding organizations, and healthcare technology solutions such as electronic health records (EHRs) and coding software.
Is continuous education important for accurate ICD-10 coding of PVCs and other cardiac conditions?
+Yes, continuous education is crucial for both coding professionals and healthcare providers. It ensures that they stay updated on the latest codes, clinical practices, and any changes to coding guidelines or conventions, ultimately leading to more accurate coding and better patient care.
How does accurate ICD-10 coding impact patient care and healthcare statistics?
+Accurate ICD-10 coding directly impacts patient care by influencing treatment decisions and ensuring that patients receive appropriate care for their conditions. It also affects healthcare statistics by providing accurate data on disease prevalence, treatment outcomes, and healthcare utilization, which can inform public health policy and resource allocation.
